What is Brainspotting? A Trauma Therapist’s Guide to How It Works and When It Helps
What Brainspotting Is and Why Therapists Go Looking for It
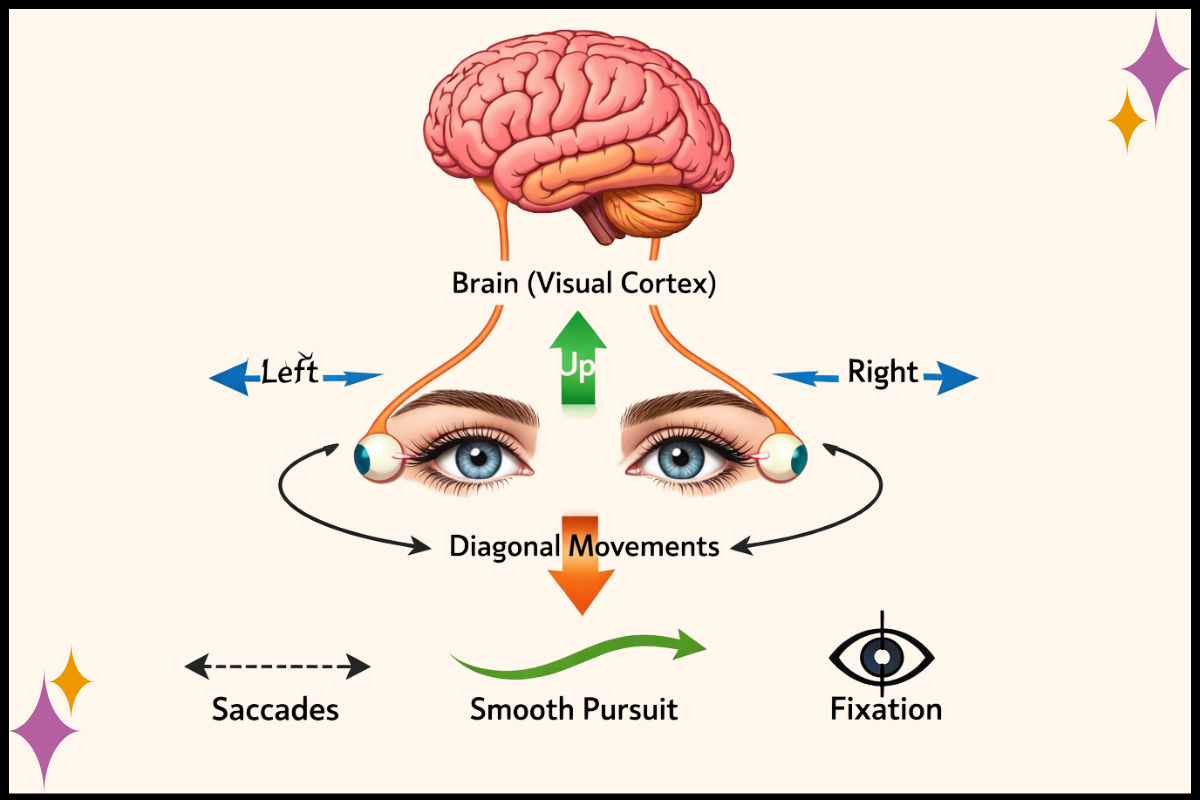
Brainspotting is a trauma therapy that helps people process stress and trauma by using eye position (where you’re looking) to access parts of the brain and nervous system where those experiences are stored.
What exactly does that mean? Well, trauma is experienced, processed, and stored in the subcortical parts of our brain (the lower parts of our brain, underneath our smart neocortex that does all the conscious thinking and processing. More on that in this video).
Because Brainspotting helps us access those lower, unconscious parts of the brain, many therapists and clients start looking into Brainspotting at a familiar point in the work - insight has happened, patterns make sense, coping skills are there, and still, something feels stuck.
Reactions feel bigger than the present moment because the body hasn’t quite caught up to what the mind understands.
This blog is here to explain what Brainspotting actually looks like in practice, how it works in the room, and when it’s often a helpful addition to trauma therapy.
How Brainspotting Was Developed
Brainspotting was developed by David Grand, PhD, a trauma therapist and early EMDR trainer who developed his own approach to EMDR, called Natural Flow EMDR.
In his work, he started noticing consistent emotional and physiological responses when clients’ eyes rested in certain positions. Rather than moving past those moments, the work evolved by paying close attention to them.
Brainspotting shares this lineage with EMDR through David’s work and background, but it became its own approach because the pacing, structure, and clinical stance are different. Where some trauma therapies are more directive or structured, Brainspotting is slower and more internally guided, with a strong emphasis on nervous system regulation and therapist attunement.
This matters because Brainspotting isn’t built on theory alone. It’s grounded in clinical observation, trauma neuroscience, and what happens when the nervous system is given space to process without being pushed.
What Actually Happens in a Brainspotting Session
One of the biggest sources of confusion about Brainspotting is not knowing what it actually looks like in session.
In a Brainspotting session, the therapist helps the client identify a “brainspot,” which is an eye position connected to emotional or physical activation (feeling tension in the body, tears welling up, racing thoughts, etc.). Finding the brainspot is often done using a pointer that the therapist moves slowly through the client’s visual field while tracking nervous system cues.
Once a brainspot is identified, the client holds their gaze in that position. From there, the work shifts into noticing using Focused Mindfulness. In this process, the client just notices what happens without judging it, and allowing whatever happens to happen.
Clients may become aware of physical sensations, emotions, images, memories, or subtle internal shifts. Sometimes things move quickly, other times they move slowly.
There’s no “right” or “wrong” way to do this part as a client.
Which, yes, can be confusing, frustrating, strange at first, but allowing the process to happen is truly crucial to the incredible outcomes we see with Brainspotting.
And with this, there is often less talking than in more traditional forms of therapy, which again doesn’t mean less is happening. Processing is unfolding at the level of the nervous system, not through problem-solving or narrative alone.
Attunement Is the Core Intervention
With all this quiet and “trust the process stuff”, you might be asking what is actually happening?
Attunement between the therapist and client ultimately is the intervention.
Yes, there are formal setups and the therapist is doing so many things in any given Brainspotting session. But most importantly, the therapist is deeply present and actively tracking the client’s nervous system moment by moment.
This includes changes in breath, muscle tension, facial expression, emotional tone, and overall regulation (among so many others). And the therapist isn’t watching from the outside. They’re co-regulating with the client throughout the session.
Rather than directing the process or pushing toward any particular outcome, the therapist supports what the client’s nervous system is already trying to do. This level of attunement is skilled, demanding work, and it’s central to why Brainspotting can access material that stays out of reach in purely cognitive approaches.
Trauma doesn’t resolve simply because we understand it. It resolves when the nervous system is able to metabolize and release what’s been held.
When “My Head Gets It, But My Body Doesn’t” Shows Up
Many people come to Brainspotting after doing meaningful work in other trauma therapies.
They understand what happened to them
They understand their symptoms
They may even be functioning better in daily life.
And yet, something still feels unresolved.
This moment is not a failure of therapy. It’s often a sign that the work is moving from cognitive understanding into deeper nervous system integration. Brainspotting is frequently used as an adjunct at this stage, offering another way to support processing without replacing what’s already been helpful.
It gives the nervous system another way in.
What This Work Asks of the Therapist
Brainspotting can be regulating and grounding work, and it can also be demanding. Sustained attunement requires the therapist’s nervous system to stay present, flexible, and regulated.
This is one reason why consultation, pacing, and community matter so much for trauma therapists when doing this kind of work. Therapists are not meant to hold this level of presence alone, session after session, without support.
How we care for the therapist’s nervous system directly impacts how sustainable this work is over time.
Brainspotting as One Option in a Larger Trauma Treatment Toolbox
Brainspotting is one trauma treatment option among many. It’s not better than other approaches, and it’s not a fit for everyone.
Some clients want structure. Some want more cognitive frameworks. Some benefit from exposure-based work. Others need slower, more internally guided approaches. The same is true for therapists.
Choosing modalities is not about allegiance. It’s about fit, capacity, and the season of practice you’re in and knowing how to pick a modality.
Trauma Lives in the Nervous System, So Does the Therapist
Trauma doesn’t live only in thoughts or memories. It lives in the nervous system.
So does healing and so does the therapist.
Brainspotting offers a way to support that level of processing through attunement, connection, and pacing, rather than forcing resolution or outcomes.
If you’re exploring trauma treatment options, this blog is part of a larger series designed to help you understand what’s available so you can make informed, grounded decisions without getting swept up in certainty or hype.
And if you’re a trauma therapist reading this, you don’t have to carry the weight of this work alone.